“Bad Cholesterol” - The Truth About LDL
For decades, we’ve been told that LDL (low-density lipoprotein) is the bad cholesterol and is what causes atherosclerosis, or “clogged arteries”. This is a gross oversimplification and is not accurate. So if you have a blood panel and find out that you have high LDL, it may not necessarily be bad, more assessment has to happen.
The plumbing analogy is usually used to describe what happens in an artery. The misconception is that heart attacks and strokes are caused by a clogged pipe. Pouring drano down the pipe should clear it out. What is really happening is that vegetable oils and sugars are more like pouring a corrosive acid down the pipe and it damages the pipe walls. Then a fragment breaks off and that is what causes heart attacks and strokes.
For those that don’t like chemistry, I’ll cut right to the chase. LDL is a transport molecule and is not what causes atherosclerosis. When the LDL molecule or its components get damaged, that is when there is cause for concern. It’s a bit like a bunch of drunk guys damaging some property, then the cops show up and blame the cab driver that brought them there. We don’t have it quite right.
Blood Panels don’t measure cholesterol, they measure lipoproteins. Lipoproteins are transport molecules, moving cholesterol from the liver to the bloodstream and back. LDL picks up cholesterols in the liver and becomes a ‘full bus’, dropping off cholesterol to various parts of the body. HDL (high-density lipoprotein) returns as an empty bus that returns to the liver to pick up cholesterol. This is a simplification and there are other states of lipoproteins but is important to note that cholesterol is vital to life. It is just that LDL has been associated with heart disease in observational studies, but these studies don’t tell the whole story.
All humans and animals produce LDL. So why, from an evolutionary perspective, does it make sense that the body would produce something that is just bad for us. It doesn’t quite add up. Could it be that there is something else at play?
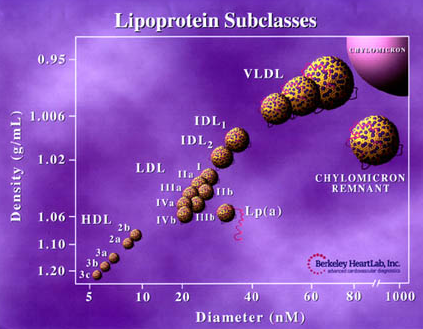
One of the persistent ideas with lipoproteins is that the size matters. The smaller they are, the more dangerous because they can infiltrate the blood vessels, or so the theory goes. However there is a flaw in that logic, as even the smallest LDL molecules are bigger than the HDL (so called ‘good’ cholesterol). See the chart below:
We used to look at total cholesterol and we were concerned with getting that number down. Then we broke it into HDL (good) and LDL (bad). The LDL category can be broken into two subcategories, either a healthy (stable) or unhealthy (unstable) molecule. If it is healthy, there are no negative effects. If it is damaged, then it can begin to line the arteries. What damages it? Oxidation. Oxidation is what happens to bananas and apples when left out. These are fruits that are low in antioxidants and aren’t able to prevent oxidation well. Oxidation at the organic level can modify and damage molecules and cause them to become unstable and behave differently.
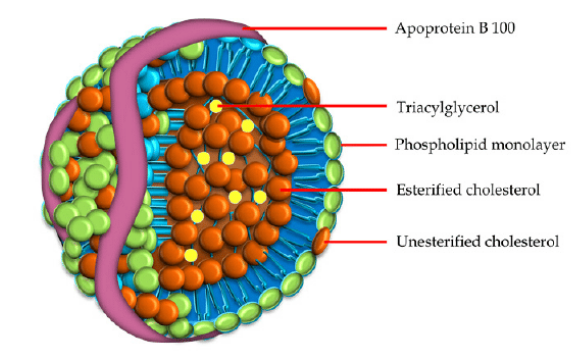
Before we get into what causes oxidation, first we have to understand the LDL molecule. Fats do not dissolve in water so they need a vehicle to move them into cells where they are supposed to go. An LDL molecule has a membrane that encases fats, and has proteins in the membrane. The one we care about for this article is called apoprotein B, or apoB for short. It’s important because when the LDL molecule reaches a cell, it recognizes apoB and allows the molecule to be taken into the cell to do its job. Without it, the LDL molecule would just circulate in the bloodstream.
When LDL molecules and their components get oxidized, they have one of two fates. When they are only minimally modified, they are still recognized by cells and are allowed in (Dinicolantonio & O’Keefe, 2018). Now they can inhibit enzymatic activity and damage the cell. When the apoB proteins are modified, now the receptors of the cell no longer recognize the LDL and block it from entry. This keeps it in circulation and attracts white blood cells since the immune system sees it as a threat. The white blood cells secrete other inflammatory mediators and all this damages the arterial wall. Then ruptures start to occur in the wall and blood clots there to prevent you from bleeding to death. It does its job in that regard but all it takes is a clot to break off to give you a heart attack or stroke (Malhotra et al., 2016).
How are these LDL molecules damaged? Simple sugars and vegetable oils (polyunsaturated fatty acid, or PUFAs for short). Sugar minimally modifies LDL through oxidation (Prasad et al., 2014). Vegetable oils are produced by extracting oil from a seed or vegetable like corn. They have to be exposed to high levels of heat for extraction. This process makes the PUFAs unstable and when they come into contact with LDL, it causes oxidative stress to the molecule. In particular, it affects the apoB protein so that cell receptors don’t recognize the molecule and now the molecule is circulating in the bloodstream. It can’t stay in circulation for eternity, so it now becomes embedded in arterial walls. Historically, vegetable oil enriched foods like margarine, have been recommended to reduce LDL. But they do that by reducing circulating LDL by leaving a fatty streak (Ganesan et al. 2019) in your artery which is obviously the opposite of what you want.
In short, saturated fat makes your cholesterol rise, but oxidation is what makes it go bad. At all costs, avoid industrially processed vegetable oils and refined sugars.
References:
Dhar, I., & Prasad, K. (2014). Oxidative Stress as a Mechanism of Added Sugar-Induced Cardiovascular Disease. International Journal of Angiology, 23(04), 217-226. doi:10.1055/s-0034-1387169
Dinicolantonio, J. J., & O’Keefe, J. H. (2018). Omega-6 vegetable oils as a driver of coronary heart disease: The oxidized linoleic acid hypothesis. Open Heart, 5(2). doi:10.1136/openhrt-2018-000898
Ganesan, R., Henkels, K. M., Wrenshall, L. E., Kanaho, Y., Paolo, G. D., Frohman, M. A., & Gomez-Cambronero, J. (2018). Oxidized LDL phagocytosis during foam cell formation in atherosclerotic plaques relies on a PLD2-CD36 functional interdependence. Journal of Leukocyte Biology, 103(5), 867-883. doi:10.1002/jlb.2a1017-407rr
Malhotra, A., Redberg, R. F., & Meier, P. (2017). Saturated fat does not clog the arteries: Coronary heart disease is a chronic inflammatory condition, the risk of which can be effectively reduced from healthy lifestyle interventions. British Journal of Sports Medicine, 51(15), 1111-1112. doi:10.1136/bjsports-2016-097285