Pronator Teres Syndrome and Numbness in Your Fingers
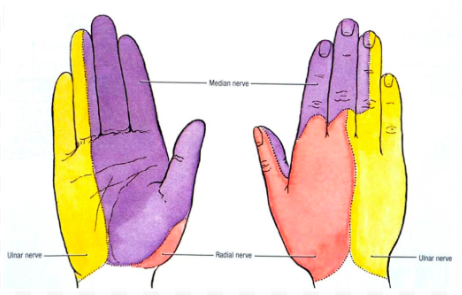
If you have numbness and tingling in your thumb, index finger, and middle finger, your median nerve is being compressed. Dermatome charts make it easy to determine which nerve is being compressed, but the difficult part is determining where the nerve is being compressed. A dermatome chart is a map of the body which depicts the areas that nerves innervate. The median nerve is the most commonly affected and is in purple in the picture below.
Nerves can be compressed from the spine, tight muscles that they pass under or through, under connective tissue or ligaments, and along joints where they take sharp turns. The most common sites of compression are the neck and the wrist. The elbow is an area of compression that is often overlooked. There are multiple areas in the elbow that can cause compression but there is a muscle that is usually the culprit: pronator teres. The pronator teres is a two headed muscle like the biceps. It crosses over the elbow in an oblique orientation which gives the muscle the ability to pronate the hand. The median nerve passes between the two heads of pronator teres where it can get pinched.
Any type of activity that requires repetitive pronation of the forearm can cause an overuse and lead to media nerve compression. Pronation is a rotational movement; think of extending your hand out for a handshake then turning your palm down. Human movement is complex and you are rarely only doing one movement at a time, rather you maybe combining pronation with other forearm movements without realizing it. Some activities that commonly cause pronator teres syndrome are prolonged hammering, ladling food, cleaning dishes, and tennis (Dididze & Sherman, 2019). There is a branch off of the median nerve called the anterior interosseous nerve which supplies the thumb, index and middle finger so it is common to have weakness and difficulty pincing objects.
To address pronator teres syndrome, the movement that is provoking it should be avoided. Massage/manual therapy will help decrease tone in the muscle. There are exercises that can be performed that will elongate the muscle and decrease entrapment of the median nerve.
The rest of this article dives into the specifics of other diagnoses that have to be ruled out to correctly diagnose pronator teres syndrome and is probably only of interest to physical therapists. The take home message is that it can be difficult to self diagnose nerve compression syndrome, but physical therapy can accurately identify and treat these conditions with good success rates.
Differential Diagnosis:
There are other areas of the elbow that must be ruled out as causes of the entrapment. The ligament of struthers, the bicipital aponeurosis, and the sublimis arch of flexor digitorum superficialis muscle are all possible areas of entrapment.
The ligament of struthers forms an arch from your humerus to your elbow. Not everyone has it; you are born with it or it can be acquired later in life. Some estimates claim that only 13.5% of the population have it (Siguiera & Martins, 2005). The median nerve passes under the arch and can be compressed. Symptoms are provoked with supination and elbow extension. The radial pulse may be diminished as well as the brachial artery can also be compressed (Dididze & Sherman, 2019).
The bicipital aponeurosis is fascia that attaches the bicep to the ulna and the median nerve courses underneath it. If this is the site of compression, symptoms would be reproduced with resisted elbow flexion with the forearm in supination (Dididze & Sherman, 2019).
The sublimis arch of the flexor digitorum is a piece of fibrous band near the origin of the muscle that controls finger flexion. If this is the source of compression, pain will be reproduced with resisted flexion of the interphalangeal joint of the middle finger while the other fingers are held in extension (Dididze & Sherman, 2019).
Because of overlapping symptoms of median nerve compression, carpal tunnel syndrome is often wrongly diagnosed. One key difference is that in pronator teres syndrome, paresthesia (numbness/tingling) will be felt through the entire dermatome. With carpal tunnel syndrome, the thenar eminence (meaty part under your thumb) will have normal sensation because the nerve that supplies this area does not pass through the carpal tunnel (Dididze & Sherman, 2019). This is especially important to determine and carpal tunnel syndrome often is sent for surgery.
There is yet another syndrome, AIN (anterior interosseous nerve) syndrome, that has a similar set of symptoms. In both AIN and pronator teres syndrome, pronation provokes pain. The key difference in testing is elbow flexion. With the elbow flexed, the pronator teres does not contribute to pronation. In other words pronation with elbow extension=pronator teres syndrome, and pronation with elbow flexed=AIN syndrome. Another key difference is that in AIN syndrome, sensation is preserved (Dididze & Sherman, 2019).
Accurate diagnosis is vital to patient outcomes. If correctly diagnosed, most patients do very well with conservative therapy. If therapy does not resolve it, corticosteroids and/or surgical decompression may be recommended.
References:
Dididze, M. and Sherman, A. (2019). Pronator Teres Syndrome. [online] Ncbi.nlm.nih.gov. Available at: https://www.ncbi.nlm.nih.gov/books/NBK526090/ [Accessed 29 Oct. 2019].
RS, S. (2019). The controversial arcade of Struthers. - PubMed - NCBI. [online] Ncbi.nlm.nih.gov. Available at: https://www.ncbi.nlm.nih.gov/pubmed/15967222 [Accessed 29 Oct. 2019].